Fracture ppt
- 1. Fracture
- 2. Introduction • Break in the structural continuity of a bone • If the overlying skin remains intact - closed (simple fracture) • If skin or one of the body cavities is breached- open (compound fracture)
- 3. Types of Fracture • Divided in to – Complete – Incomplete
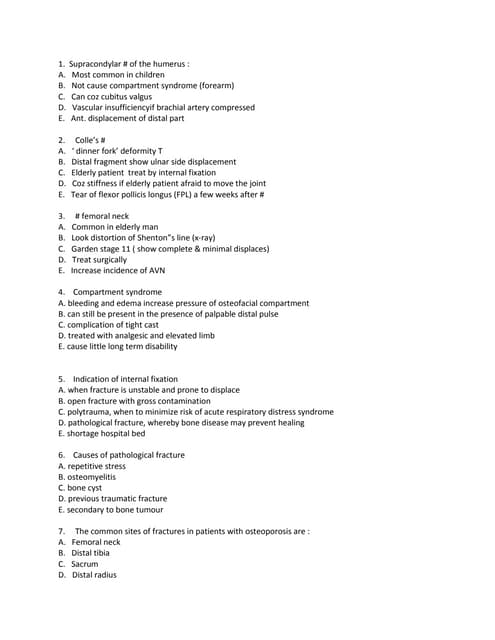
- 4. Complete fracture Bone is split into two or more fragments. The fracture pattern on x-ray can help predict behaviour after reduction • in a transverse fracture the fragments usually remain in place after reduction • if it is oblique or spiral, they tend to shorten and re- displace even if the bone is splinted. • In an impacted fracture the fragments are jammed tightly together and the fracture line is indistinct. • A comminuted fracture is one in which there are more than two fragments
- 5. Complete fractures: (a) transverse; (b) segmental and (c) spiral
- 6. Incomplete fracture • The bone is incompletely divided and the periosteum remains in continuity • Greenstick fracture : bone is buckled or bent – Mainly seen in children, because of their springy bones – Plastically deformed bones • Compressed fracture: crumpled cancellous bone – Seen in adults, mainly in vertebral bodies, calcaneum and tibial plateu
- 7. Incomplete fractures: (a) buckle or torus and (b,c)) greenstick.
- 8. Muller’s Classification (a) Each long bone has three segments – proximal Diaphyseal Distal the proximal and distal segments are each defined by a square based on the widest part of the bone. (b,c,d) Diaphyseal fractures may be simple wedge complex. (e,f,g) Proximal and distal fractures may be extra-articular, partial articular complete articular.
- 9. How fractures are displaced • Fractures can be displaced by: – Force of the injury – Effects of gravity – Pull of muscles attached to the site
- 10. Types of displacement • Translation (shift)- the fragments may shift sideways, backwards or forwards • Angulation (tilt)- mal alignment if unconnected will lead to limb deformity • Rotation (twist)- rotational deformity • Length- can cause shortening of the bone
- 11. Mechanism of injury • Injury • Repetitive stress • Pathological fractures
- 12. • INJURY o Direct force- With a direct force, the bone breaks at the point of impact; the soft tissues also are damaged. o Indirect force-the bone breaks at a distance from where the force is applied.
- 13. Some fracture patterns reveals the dominant mechanism: Spiral pattern- twisting Oblique- compression Triangular- bending Transverse- tension
- 14. Some fracture patterns suggest the causal mechanism: (a) spiral pattern (twisting); (b) short oblique pattern (compression); (c) triangular ‘butterfly’ fragment (bending) and (d) transverse pattern (tension). Spiral and some (long) oblique patterns are usually due to low-energy indirect injuries; bending and transverse patterns are caused by high-energy direct trauma.
- 15. • FATIGUE OR STRESS FRACTURES- Occur in normal bone, subject to repeated heavy loading, typically in athletes, dancers or military personnel. Drugs like steroids and methotrexate
- 16. • PATHOLOGICAL FRACTURES- Occurs in a bone that is made weak by some disease. Causes- Inflammatory- Osteomyelitis Neoplastic- giant cell tumour, Ewings sarcoma, secondaries
- 17. Miscellaneous bone conditions- simple bone cyst, anuerysmal bone cyst Heriditary- Osteogenesis imperfecta, Osteopetrosis Other acquired generalised diseases- Osteoporosis, osteomalacia, rickets
- 18. BONE HEALING • PRIMARY FRACTURE HEALING refers to fractures treated operatively without callus formation • SECONDARY FRACTURE HEALING refers to (a) fractures treated non-operatively, with the formation of callus and no disturbance of hematoma; (b) fractures operated without disturbance of hematoma
- 19. FACTORS AFFECTING BONE HEALING (A)Age: Fractures unite faster in children (B)Type of bone: Faster union in flat and cancellous bone (C)Pattern of fracture: Spiral # > oblique # > transverse # > comminuted # (D)Disturbed pathoanatomy: soft tissue interposition and ischaemic # prevent faster healing
- 20. (E)Type of reduction: good apposition of fracture results in faster healing (F)Immobilisation: depends on the fracture site eg. Fracture ribs and scapula do not require immobilisation (G)Open fractures: often go into delayed union and non-union (H)Compression of fracture site: enhances union(cancellous bone) and primary bone healing(cortical bone)
- 21. HEALING BY CALLUS • STAGE 1: TISSUE DESTRUCTION AND HEMATOMA FORMATION - lasts for 7 days - blood leaks out of torn vessels and forms a hematoma between and around fracture - periosteum and local soft tissues are stripped off - ischaemic necrosis – death of some osteocytes with sensitization of the remaining precursor cells
- 22. • STAGE 2: INFLAMMATION AND CELLULAR PROLIFERATION/GRANULATION TISSUE - lasts for 2-3 weeks - precursor cells form cells that differentiate and organize to provide q vessels, fibroblasts, osteoblasts etc - soft granulation tissue formed between fracture fragments, providing anchorage to fracture - hematoma is slowly absorbed and fine new capillaries grow into the area
- 23. • STAGE 3: CALLUS FORMATION - lasts for 4-12 weeks - granulation tissue differentiates and creates osteoblasts, laying down intercellular matrix impregnated with calcium salts - formation of callus/woven bone - provides good strength to the fracture, decreasing the movements at the fracture site and causes union in about 4 weeks
- 24. • STAGE 4: REMODELLING - takes 1-4 years for the bone to become strong enough to carry weight - with continuing osteoclastic and osteoblastic activities, the woven bone gets transformed into lamellar bone - osteoblasts fill in the remaining gap between the new bone and the fragments to strengthen the bone
- 25. • STAGE 5: MODELLING - stage where the bone is gradually strengthened - shapening of the cortices occurs at the endosteal and periosteal surfaces - all these occur when the person starts resuming his activities ie bearing weight and muscle forces - thicker lamellae are laid down where high stresses are present, unwanted buttresses are carved away and medullary cavity is reformed
- 26. HEALING BY DIRECT UNION • Formation of callus requires stimulus from movement • In cases of impacted fracture in cancellous bone or a fracture immobilised by the use of metal plate, callus will not be formed and hence the fracture will heal by direct union
- 27. 1. Osteoblastic new bone formation occurs directly between the fracture fragments 2. New capillaries and osteoprogenitor cells grow in from the edges and lay down new bone on the exposed surface (gap healing) 3. Lamellar bone is produced in the narrow crevices (<200μm) while woven bone is produced in the wider gaps which is then remodelled into lamellar bone
- 28. 4. Penetration and bridging of the fracture by osteoclasts and osteoblasts in 3-4 weeks. 5. Intimacy of the contact surfaces lead to internal bridging without intermediate stages (contact healing)
- 29. CLINICAL PRESENTATION OF FRACTURES
- 30. In the Casualty.. • Take a Brief History. • General Particulars: • AGE & SEX Children and the elderly Different mechanisms of injury : Traumatic , Pathological Post menopausal women : Osteoporosis and pathological fractures. • HISTORY OF TRAUMA – Ascertaining the mechanism of injury is important, helps understand symptoms and aids examination.
- 31. SYMPTOMS • A history of injury, followed by inability to use the injured limb. The fracture may not always be at the site of the injury. • Eg : A blow to the knee and its varied effects. If a fracture occurs with trivial trauma, or spontaneously, suspect a pathological lesion. • Pain • Bruising • Swelling These are common symptoms but they do not distinguish a fracture from a soft-tissue injury.
- 32. • Deformity – More suggestive of a fracture. • Enquire about symptoms of associated injuries: Pain and swelling elsewhere (it is a common mistake to get distracted by the main injury, particularly if it is severe), Numbness or Loss of movement. Skin pallor or cyanosis. Blood in the urine. Abdominal pain. Difficulty with breathing. Transient loss of consciousness. • Ask about previous injuries, or any other musculoskeletal abnormality that might cause confusion when the x-ray is seen. Finally, a general medical history is important, in preparation for anaesthesia or operation.
- 33. GENERAL SIGNS • First follow the ABCs: look for, and if necessary attend to, • Airway obstruction, • Breathing problems, • Circulatory problems • Cervical spine injury. • Secondary survey – Examine the main injury- ascertain the type of fracture, classify, plan a management protocol and look out for complications. • It will also be necessary to exclude other previously unsuspected injuries.
- 34. LOCAL SIGNS • Familiar headings of clinical examination should always be considered, • (or damage to arteries, nerves and ligaments may be overlooked.) • A systematic approach is always helpful: Examine the most obviously injured part. Test for artery and nerve damage. Look for associated injuries in the region. Look for associated injuries in distant parts.
- 35. LOOK • For Swelling, bruising and deformity • Examine whether the skin is intact • Note also the posture of the distal extremity and the colour of the skin.
- 36. FEEL • The injured part is gently palpated for localized tenderness. • The common and characteristic associated injuries should also be felt for, even if the patient does not complain of them. • Vascular and peripheral nerve abnormalities should be tested for both before and after treatment.
- 37. MOVE • Crepitus and abnormal movement may be present. • More important to ascertain if the patient can move the joints distal to the injury.
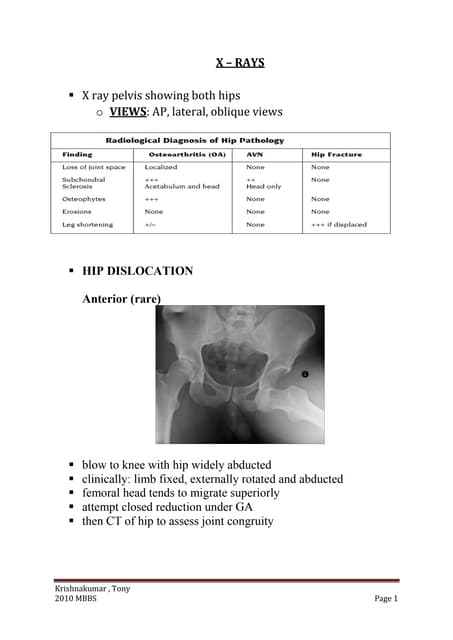
- 38. X-RAY INVESTIGATION • X-ray examination is mandatory. • Rule of twos: Two views – A fracture or a dislocation may not be seen on a single x-ray film, and at least two views (anteroposterior and lateral) must be taken. Two limbs – In children, the appearance of immature epiphyses may confuse the diagnosis of a fracture; x- rays of the uninjured limb are needed for comparison.
- 39. Two films of the same tibia: the fracture may be ‘invisible’ in one view and perfectly plain in a view at right angles to that.
- 40. Two limbs: Sometimes the abnormality can be appreciated only by comparison with the normal side; in this case there is a fracture of the lateral condyle on the left side R L
- 41. Two joints – In the forearm or leg, one bone may be fractured and angulated. Angulation, however, is impossible unless the other bone is also broken, or a joint dislocated. The joints above and below the fracture must both be included on the x- ray films. Two injuries – Severe force often causes injuries at more than one level. Eg: In fractures of the calcaneum or femur it is important to also x-ray the pelvis and spine. Two occasions – Some fractures are notoriously difficult to detect soon after injury, but another x-ray examination a week or two later may show the lesion. Eg: Undisplaced fractures of the distal end of the clavicle, scaphoid, femoral neck and lateral malleolus, and also stress fractures and physeal injuries.
- 42. Two joints: The first x-ray (1) did not include the elbow. This was, in fact, a Monteggia fracture – the head of the radius is dislocated; (2) shows the dislocated radiohumeral joint.
- 43. More than one occasion: A fractured scaphoid may not be obvious on the day of injury, but clearly seen 2 weeks later.
- 44. SPECIAL IMAGING • Computed tomography (CT) may be helpful in lesions of the spine or for complex joint fractures; help in accurate visualization of fractures in ‘difficult’ sites such as the calcaneum or acetabulum. • Magnetic resonance imaging (MRI) may be the only way of showing whether a fractured vertebra is threatening to compress the spinal cord. • Radioisotope scanning is helpful in diagnosing a suspected stress fracture or other undisplaced fractures.
- 45. FINAL DESCRIPTION • Diagnosing a fracture is not enough; the surgeon should describe it with its properties: • Is it open or closed? • Which bone is broken, and where? • Has it involved a joint surface? • What is the shape of the break? • Is it stable or unstable? • Is it a high-energy or a low-energy injury? In short, the examiner must learn to recognize what has been aptly described as the ‘personality’ of the fracture.
- 46. Complications of Fracture
- 47. VISCERAL INJURIES
- 48. • Often occur in fractures around the trunk • Penetration of lung by rib fractures which causes pneumothorax • Rupture of bladder or urethra in pelvic fractures • Require emergency treatment
- 49. VASCULAR INJURY
- 50. Injury Vessel First rib fracture Subcalvian Shoulder dislocation Axillary Humeral supracondylar fracture Brachial Elbow dislocation Brachial Pelvic fracture Presacral and internal iliac Femoral supracondylar fracture Femoral Knee dislocation Popliteal Proximal tibial Popliteal or its branches
- 51. Clinical features • Paraesthesia or numbness • Injured limb is cold and pale or slightly cyanosed • Weak or absent pulse
- 52. Treament • All bandages and splints should be remove • Fractures re-x-rayed and if artery is being compressed prompt reduction is required • Circulation reassessed repeatedly over the next half hour • If no improvement, vessels must be explored by operation with pre or peroperative angiography
- 53. • Cut vessel can be sutured, or a segment may be replaced by a vein graft, if it is thrombosed, endarterectomy may restore blood flow • If vessel repair is done, stable fixation is a must and fracture should be fixed internally
- 54. NERVE INJURY
- 55. Injury Nerve Shoulder dislocation Axillary Humeral shaft fracture Radial Humeral supracondylar fracture Radial or median Elbow medial condyle Ulnar Moteggia fracture-dislocation Posterior-interosseous Hip dislocation Sciatic Knee dislocation peroneal
- 56. Closed nerve injuries • Seldom severe and spontaneous recovery occurs in 90% within 4 months • Nerve should be explored if no recovery, nerve conduction studies and EMG fail to show evidence of recovery
- 57. Open nerve injuries • Nerve should be explored at the time of debridement and repair at the time or at wound closure
- 58. Acute nerve compression • Sometimes occurs with # or dislocations around the wrist • Numbness or paraesthesia in distribution of the median or ulnar nerves • # reduction or splitting of bandages around the splint • If no improvement within 48 hours, nerve should be explored and decompressed
- 59. • Indications for early exploration 1. Associated with open # 2. Fractures that need internal fixation 3. Presence of concomitant vascular injury 4. Diagnosed after manipulation of the #
- 60. HAEMARTHROSIS
- 61. • # involving joint • Joint is swollen, tense and patient resist any attempt at moving at • Blood should be aspirated before dealing with #
- 62. INFECTION
- 63. Early infection • May present as wound inflammation without discharge • Causal organism 1. S. aureus 2. Pseudomonas • Antibiotics may allow # to proceed to union as long as fixation remains stable • But further surgery is likely later, when antibiotics are stopped
- 64. Late presentation • May present with a sinus and xray evidence of sequestra • Implants and all avascular pieces of bone should be removed • External fixator can be used to bridge the # • If resulting defect too large for bone grafting, patient should be referred to a limb reconstruction centre
- 65. • When infection involves a joint, principles of treatment are the same as with bone infection, namely debridement and drainage, drugs and splintage • On resolution of infection, # is stabilize so that joint movement can recommence • If # cannot be stablized, joint should be splinted in the optimum position • Can lead to permanent stiffness
- 66. Compartment Syndrome • Occurs with fracture of elbow, forearm bones, proximal third of tibia, hands or foot ; • Crush injuries and circumferential burns • Increase of pressure within the osseofascial compartment • Due to bleeding , oedema or inflammation
- 67. • Clinical features – Pain : bursting sensation – Altered sensibility – Paresis / weakness in active muscle contraction – Testing the muscle by stretching them ( ischemic muscle is highly sensitive to stretch and it causes pain )
- 68. • Confirmation of diagnosis – Measuring the intracompartmental pressures • Introduced a split catheter into the compartment • Pressure measured close to level of the fracture • Differential pressure (difference between the diastolic pressure and compartment pressure ) is <30mmHg – immediate decompression • Management – Remove any casts, bandages and dressings – Differential pressure < 30mmHg – immediate fasciotomy
- 69. Gas gangrene • Produced by Clostridial infection • Present in dirty wound with dead muscle that are closed without adequate debridement • Toxins can cause necrosis of tissue and promote the spread of the disease
- 70. • Clinical features – Within 24 hours of injury – Intense pain – swelling around the wound – Brownish discharge – Little or no pyrexia – Increase pulse rate – Characteristic smell – Patient rapidly become toxemia and may lapse into coma and death
- 71. • Prevention – All dead tissue should be completely excised – Doubt about tissue viability – wound should be left open • Treatment – Early diagnosis – Fluid replacement & IV antibiotics – Hyperbaric O2 – limit the spread of gangrene – Prompt decompression of the wound and removal of dead tissue – Amputation in advance cases
- 72. Fracture Blisters • 2 types – Clear fluid filled vesicles – Blood stained • Occur during limb swelling • Due to elevation of the epidermal layer of the skin from the dermis • No advantage in puncturing the blister ( cause local infection ) • Surgical incision can be done after the limb swelling decrease
- 73. Plaster and Pressure Sores • Occur where the skin presses directly onto bone • Traction on a Thomas Splint ( wrong ring size, excessive fixed traction and neglect) • Prevention – Padding the bony points – Moulding the wet plaster so that pressure is distributed to the soft tissue around the bony points
- 74. • Treatment – Patient feels the localised burning pain ( warning sign ) – Window must be immediately cut in the plaster – If unnoticed, skin necrosis will progress
- 75. LATE COMPLICATIONS DELAYED UNION When a fracture takes more than usual time to unite, it is said to have gone in ‘delayed union’.
- 76. Causes Factors causing delayed union can be summarized as: biological, biomechanical or patient-related. BIOLOGICAL --Inadequate blood supply --Severe soft tissue damage affects fracture healing by: (1) reducing the effectiveness of muscle splintage (2) damaging the local blood supply and (3) diminishing or eliminating the osteogenic input from mesenchymal stem cells within muscle --Periosteal stripping
- 77. BIOMECHANICAL --Imperfect splintage --Over-rigid fixation --Infection PATIENT RELATED In a less than ideal world, there are patients who are: • Immense • Immoderate • Immovable • Impossible. These factors must be accommodated in an appropriate fashion.
- 78. Clinical features -Fracture tenderness persists -Pain may be acute -On x-ray- fracture line remains visible - there is very little or incomplete callus formation or periosteal reaction - However, the bone ends are not sclerosed or atrophic (suggest that, although the fracture has not united, it eventually will)
- 79. Treatment Conservative principles are: (1) to eliminate any possible cause of delayed union (2) to promote healing by providing the most appropriate environment Immobilization (whether by cast or by internal fixation) should be sufficient to prevent shear at the fracture site, but fracture loading is an important stimulus to union and can be enhanced by: (1) encouraging muscular exercise (2) by weightbearing in the cast or brace
- 80. OPERATIVE --If union is delayed for more than 6 months and there is no sign of callus formation, internal fixation and bone grafting are indicated.
- 81. NON-UNION Delayed union gradually turns into non-union – that is it becomes apparent that the fracture will never unite without intervention Movement can be elicited at the fracture site and pain diminishes; the fracture gap becomes a type of pseudoarthrosis. This patient has an obvious pseudarthrosis of the humerus. The X-ray shows a typical hypertrophic non union
- 82. X-ray -The fracture is clearly visible but the bone on either side of it may show either exuberant callus or atrophy -This contrasting appearance has led to nonunion being divided into hypertrophic and atrophic types. -In hypertrophic non-union the bone ends are enlarged, suggesting that osteogenesis is still active but not quite capable of bridging the gap -In atrophic non-union, osteogenesis seems to have ceased
- 83. Causes Biological and patient related: (1) poor soft tissues (from either the injury or surgery) (2)local infection (3) associated drug abuse, anti-inflammatory or cytotoxic immunosuppressant medication (4) non-compliance on the part of the patient.
- 84. TREATMENT CONSERVATIVE Non-union is occasionally symptomless, needing no treatment or, at most, a removable splint with hypertrophic non-union, functional bracing may be sufficient to induce union, but splintage often needs to be prolonged. Pulsed electromagnetic fields and low-frequency, pulsed ultrasound can also be used to stimulate union.
- 85. OPERATIVE --hypertrophic non-union -- very rigid fixation alone (internal or external) may lead to union. --atrophic non-union, fixation alone is not enough. Fibrous tissue in the fracture gap, as well as the hard, sclerotic bone ends is excised and bone grafts are packed around the fracture. If there is significant ‘die-back’, this will require more extensive excision and the gap is then dealt with by bone advancement using the Ilizarov technique.
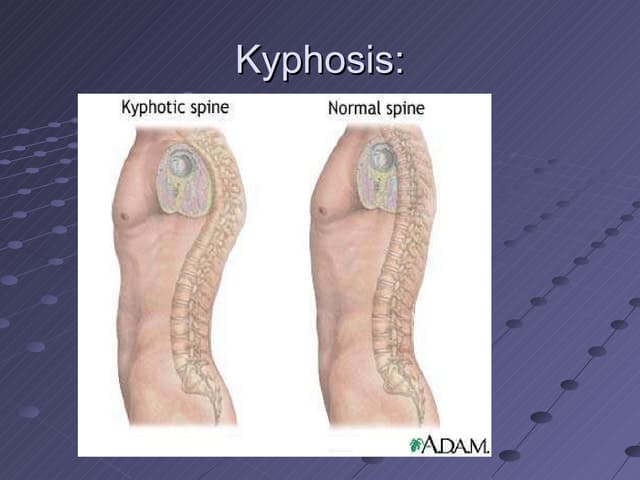
- 86. Malunion • the fragments join in an unsatisfactory position (unacceptable angulation, rotation or shortening) • Causes are : failure to reduce a fracture adequately failure to hold reduction while healing proceeds gradual collapse of comminuted or osteoporotic bone.
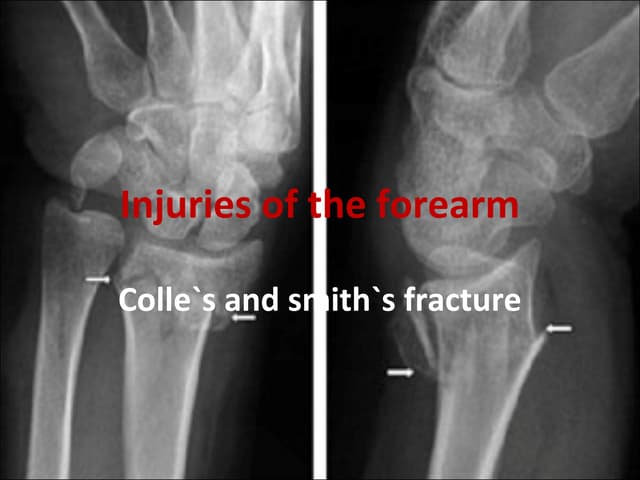
- 87. • Common sites: fractures at the ends of a bone • E.g. supracondylar fracture of the humerus, Colles fracture. • Consequences: Deformity Shortening of the limb Limitation of movements
- 88. • X-rays are essential to check the position of the fracture while it is uniting. • Important during the first 3 weeks, when the situation may change without warning.
- 89. • Treatment 1. In adults, • fractures should be reduced as near to the anatomical position as possible. • Angulation of more than 10–15 degrees in a long bone or a noticeable rotational deformity may need correction by remanipulation, or by osteotomy and fixation.
- 90. 2. In children, • angular deformities near the bone ends (and especially if the deformity is in the same plane as that of movement of the nearby joint) will usually remodel with time; • rotational deformities will not.
- 91. 3. In the lower limb, • shortening of more than 2.0 cm is seldom acceptable to the patient • a limb length equalizing procedure may be indicated.
- 92. Avascular Necrosis • Certain regions are notorious for their propensity to develop ischaemia and bone necrosis after injury • Common sites: the head of the femur (after fracture of the femoral neck or dislocation of the hip) the proximal part of the scaphoid (after fracture through its waist) the lunate (following dislocation) the body of the talus (after fracture of its neck).
- 93. • Consequences Deformation of the bone Leads to secondary osteoarthritis a few years later Painful limitation of joint movement
- 94. • X-ray shows the characteristic increase in x-ray density, which occurs as a consequence of two factors: • Disuse osteoporosis in the surrounding parts gives the impression of ‘increased density’ in the necrotic segment, • and collapse of trabeculae compacts the bone and increases its density.
- 95. • Treatment : usually becomes necessary when joint function is threatened. In old people with necrosis of the femoral head an arthroplasty is the obvious choice; in younger people, realignment osteotomy (or, in some cases, arthrodesis) may be wiser. Avascular necrosis in the scaphoid or talus may need no more than symptomatic treatment, but arthrodesis of the wrist or ankle is sometimes needed.
- 96. Growth Disturbance • In childern, due to damage to physis • Transverse fractures not dangerous as long it does run through germinal zone • Prevented by accurate reduction • Epiphysis splitting fractures -> asymmetrical growth and angulated bone ends • Complete cessation of growth – if entire physis is damaged.
- 97. Bed Sores • Elderly or Paralysed • Skin over sacrum and heels – most vulnerable • Prevention by careful nursing and early activity • Treatment is difficult. By necrotic tissue excision and skin grafting • Vacuum assisted closure for sacral sores
- 98. Myositis Ossificans • Heterotopic ossification after injury • Dislocation of elbow or blow to brachialis, deltoid or quadriceps • Pain , swelling and tenderness • Bone scan – increased activity • Limited joint movement • 8 weeks , easily palpable , defined in x ray • Immobilization, Excision, NSAIDS ,Radiotherapy
- 99. Tendon Lesions • Tendinitis – Tibialis posterior tendon after medial malleolar fractures • Rupture of EPL tendon 6-12 weeks after fracture of lower radius • Corrected by transfer of extensor indicis proprius tendon
- 100. Nerve Compression • Lateral popliteal nerve – external rotation • Radial palsy – crutches • Numbness, paraesthesia, loss of power and wasting • Ulnar, Median and Posterior tibial nerve • Decompression
- 101. Muscle Contracture • Ischaemic contractures of affected muscles • Deformity and stiffness • Forearm and hand, leg and foot • Wasting and Clawing of fingers • Due to injuries and tight bandage • Calf ischemia – popliteal artery or its divisions • Tendon transfer
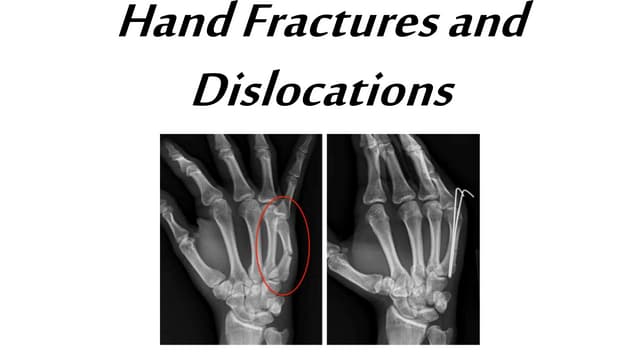
- 102. Joint Instability and Stiffness • Instability – Ligamentous laxity, muscle weakness and bone loss • Recurrent dislocation • Stiffness – knee, elbow ,shoulder ,small joints of hand • Hemarthrosis – synovial adhesions • Treatment is by exercise to prevent occurence
- 103. Sudeck’s dystrophy • Complex regional pain syndrome • Algodystrophy • Reflex sympathetic dystrophy • Type 1 – RSD develops after injurious or noxious event • Type 2 – Causalgia develops after nerve injury • Pain(burning),swelling,redness,pale skin and atrophy
- 104. • Early recognition • Elevation and active exercises • NSAIDS, regional anaesthesia • Drugs like amitriptyline, carbamazepine and gabapentin • Physiotherapy
- 105. Osteoarthritis • Damage to articular cartilage –post traumatic • Irregular joint surface – local stress • Intra – articular osteotomies and repositioning of fragment • Malunion – secondary osteoarthritis